Contents
- Executive summary for the Pharmaceutical Needs Assessment (PNA) 2025
- Section 1: Introduction
- Section 2: Context for the PNA
- Section 3: NHS pharmaceutical services provision, currently commissioned
- Section 4: Other services that may impact on pharmaceutical services provision
- Section 5: Findings from the public questionnaire
- Section 6: Analysis of health needs and pharmaceutical service provision
- Section 7: Conclusions
- Appendix A: List of pharmaceutical service providers in Bexley by locality
- Appendix B: PNA project plan
- Appendix C: PNA Steering Group terms of reference
- Appendix D: Public questionnaire
- Appendix E: Consultation stakeholders
- Appendix F: Summary of consultation responses
- Appendix G: Consultation comments
- Appendix H: List of Abbreviations
- Supplementary Statements and map updates
2. Section 1: Introduction
1.1 Background
The Health Act 2009, implemented in April 2010, mandated Primary Care Trusts (PCTs) in England to undertake and publish Pharmaceutical Needs Assessments (PNAs) within specific timeframes. These PNAs:
- inform local commissioning decisions regarding pharmaceutical services. They provide evidence of the current and future needs for pharmaceutical services in the area, helping NHS England (NHSE), local authorities, and Integrated Care Boards (ICBs) make informed decisions about service provision and commissioning
- are a key tool in determining market entry for new pharmaceutical services. They identify any gaps in service provision and help decide whether new pharmacies or service providers are needed to meet the pharmaceutical needs of the population
- can contribute to public health strategies by assessing how pharmaceutical services can support broader health initiatives, such as reducing hospital admissions, promoting healthy lifestyles, and improving access to services for vulnerable populations
- help plan for future pharmaceutical service provision, ensuring the area’s needs are met as the population grows or changes by assessing upcoming developments such as housing projects or demographic changes
The Health and Social Care Act 2012 transferred responsibility for developing and updating PNAs to Health and Wellbeing Boards (HWBs). PNAs are a statutory requirement, and they must be published in accordance with the NHS (Pharmaceutical Services and Local Pharmaceutical Services) Regulations 2013 (hereafter referred to as the Pharmaceutical Regulations 2013).
The Pharmaceutical Regulations 2013 were last updated in 2013 (SI 2013/349)1 and came into force on 1 April 2013.
The initial PNAs were published in 2011 (see Table 1 for timelines).
| 2009 | 2011 | 2013 | 2015 | Ongoing |
|---|---|---|---|---|
| Health Act 2009 introduces statutory framework requiring Primary Care Trusts (PCTs) to prepare and publish PNAs | PNAs to be published by 1 February 2011 | The Pharmaceutical Regulations 2013 outline PNA requirements for HWBs | HWBs required to publish own PNAs by 1 April 2015 | PNAs reviewed every 3 years* |
*Publication of PNAs was delayed during C-19 pandemic and PNAs were published by October 2022.
This assessment should be revised within three years of its previous publication. The last PNA for Bexley HWB was published in September 2022. This PNA for Bexley HWB fulfils this regulatory requirement.
1.2 Important changes since the last Pharmaceutical Needs Assessment (PNA)
There was an update to the Pharmaceutical Regulations 2013 in May 2023, which, in the main, was in response to the number of requests for temporary closures. Key changes were made for:
- notification procedures for changes in core opening hours
- notification procedures for 100-hour pharmacies to be able to reduce their hours to no less than 72 hours per week
- local arrangements with ICBs for the temporary reduction in hours
- all pharmacies requiring a business continuity plan that allows them to deal with temporary closures
Clinical Commissioning Groups (CCGs) are now replaced by Integrated Care Boards (ICBs) as part of Integrated Care Systems (ICSs). In an ICS, NHS organisations, in partnership with local councils and others, take collective responsibility for managing resources, delivering NHS standards and improving the health of the population they serve.
Integrated Care Boards took on the delegated responsibility for the commissioning of pharmacy services from NHS England from 1 April 2023.
The Community Pharmacy sector has reported workforce challenges and pressures reported by the National Pharmacy Association2 and Healthwatch3 . Both reports highlighted that the current rate of pharmacy closures for 2024 was higher than previous years mainly due to a combination of funding and workforce challenges. The Pharmacy pressures4 report by Community Pharmacy England based on a survey conducted in 2024 highlights the pressures in community pharmacy and morale. Key headlines based on the views of the owners of 6,100 premises:
- three quarters of pharmacy team members report staff shortages
- 1 in 10 resulting in temporary closures
- almost 92% of pharmacy staff report they are not coping well because of the workload
- three-quarters of pharmacy owners reported recruitment difficulties to hire permanent staff
Pharmacy First Service5 – The Pharmacy First service commenced on 31 January 2024 and replaces the Community Pharmacist Consultation Service (CPCS). The new Advanced service involves pharmacists providing advice and prescription-only treatment under a Patient Group Direction (PGD) or in one pathway, an over-the-counter medicine (supplied under a clinical protocol), all at NHS expense, for seven common conditions. Consultations for these seven clinical pathways can be provided to patients presenting to the pharmacy as well as those referred by NHS 111, general practices and others. The service will also incorporate the elements of the CPCS, i.e. minor illness consultations with a pharmacist and the supply of urgent medicines (and appliances), both following a referral from NHS 111, general practices and other authorised healthcare providers (i.e. patients are not able to present to the pharmacy without a referral).
Hypertension Case-Finding Service6 requirements were updated from 1 December 2023 which means the service can be provided by suitably trained and competent pharmacy staff; previously, only pharmacists and pharmacy technicians could provide the service.
Hepatitis C testing service was decommissioned from 1 April 2023.
COVID-19 and the Lateral Flow Device (LFD) service7 - The NHS offers COVID-19 treatment to people with COVID-19 who are at risk of becoming seriously ill. Prior to the introduction of this service, rapid LFD tests were available to order by these patients on gov.uk or by calling NHS 119. These kits were then delivered directly to the patient’s home. From 6 November 2023, LFD tests will no longer be available via gov.uk or via NHS 119. The objective of this service is to offer eligible at risk patients access to LFD tests to enable testing at home for COVID-19, following symptoms of infection. A positive LFD test result will be used to inform a clinical assessment to determine whether the patient is suitable for, and will benefit from, NICE recommended COVID-19 treatments.
Pharmacy Quality Scheme (PQS): The PQS is a voluntary scheme that forms part of the CPCF8. It supports the delivery of the NHS Long Term Plan (LTP) and rewards community pharmacy contractors that deliver quality criteria in three quality dimensions: clinical effectiveness, patient safety and patient experience. The PQS has been developed to incentivise quality improvement in specific areas yearly. Due to the 2024 elections, negotiations were paused and at the time of writing no details had been released. There is currently no PQS for the financial year 2024/25.
1.3 Key upcoming changes
Although the PNA was drafted in November 2024, the following changes will occur during the lifetime of this PNA. They have been considered and agreed following consultation that will not have an impact on the conclusions of this PNA. Therefore, they have been added to this document in June 2025.
An announcement was made in March 2025 which included changes to some of the services and changes to the Pharmaceutical Regulations 2013. Some of the key changes are listed below:
- PLPS Regulations amendments: Ability to change core opening hours: These amendments to the PLPS Regulations are intended to allow pharmacy owners greater flexibility in adjusting their opening hours to better align with the needs of patients and likely users. While the changes have not yet come into force, they are expected to take effect during the lifespan of this PNA
- DSPs will no longer be permitted to provide Advanced and Enhanced services on their premises, though remote provision will still be allowed where specified
- from 23 June 2025, no new applications for DSPs will be accepted, following amendments to the PLPS Regulations 2013 which close entry to the DSP market
- funding and fees: Additional funding has been allocated and agreed for the Community Pharmacy Contractual Framework for 2025/2026
Service developments:
- from October 2025, the Pharmacy Contraception Service will be expanded to include Emergency Hormonal Contraception
- New Medicine Service will be expanded to include depression from October 2025
- Childhood Flu Vaccination Service, which covers all children aged 2 and 3 years old, will be trialled as an Advanced Service for one season from October 2025
- Smoking Cessation Service will have Patient Group Directions introduced to enable provision of Varenicline and Cytisinicline (Cytisine). No dates have been given for this
In March 2025, the government decided to merge NHS England into the Department of Health and Social Care, aiming to reduce bureaucracy and improve the management of health services. A timeline for this is still being developed.
1.4 Purpose of the PNA
The ICB through their delegated responsibility from NHSE is required to publish and maintain pharmaceutical lists for each HWB area. Any person wishing to provide NHS pharmaceutical services is required to be included on the pharmaceutical list. NHSE must consider any applications for entry to the pharmaceutical list. The Pharmaceutical Regulations 2013 require the ICB to consider applications to fulfil unmet needs determined within the PNA of that area or applications for benefits unforeseen within the PNA. Such applications could be for the provision of NHS pharmaceutical services from new premises or to extend the range or duration of current NHS pharmaceutical services offered from existing premises. This function is carried out by the Dentistry, Optometry and Pharmacy Commissioning Hub hosted by NHS North East London on behalf of all London ICBs.
The PNA is the basis for the ICB to make determinations on such applications. It is therefore prudent that the PNA is compiled in line with the regulations and with due process, and that the PNA is accurately maintained and up to date. Although decisions made by the ICB regarding applications to the pharmaceutical list may be appealed to the NHS Primary Care Appeals Unit, the final published PNA cannot be appealed. It is likely the only challenge to a published PNA will be through an application for a judicial review of the process undertaken to conclude the PNA.
The PNA should be read alongside other Joint Strategic Needs Assessment (JSNA) products. Following national guidance, Bexley Council decided to adopt a more responsive and ongoing approach to the JSNA, via the Bexley Data Observatory9. Information is automatically updated from available local and national data sources, and is presented visually, with the use of health maps, infographics and charts.
The Bexley Joint Local Health and Wellbeing Strategy (JLHWS) 2023 to 202810 is informed by the above JSNA products.
The PNA assesses how pharmaceutical services meet the public health needs identified in the JSNA, both now and in the future. By informing decisions made by the local authority and the ICB, these documents jointly aim to improve the health and wellbeing of the local population and reduce inequalities.
ICBs have been given delegated responsibility for pharmacy commissioning from NHSE and therefore some services currently commissioned from pharmacies by ICBs may fall under the definition of Enhanced Services in the future. For the purpose of this PNA, at the time of writing, only services commissioned by NHSE as per the regulations have been considered as ‘NHS pharmaceutical services’.
1.5 Scope of the PNA
The Pharmaceutical Regulations 2013 detail the information required to be contained within a PNA. A PNA is required to measure the adequacy of pharmaceutical services in the HWB area under five key themes:
- necessary services: current provision
- necessary services: gaps in provision
- other relevant services: current provision
- improvements and better access: gaps in provision
- other services
In addition, the PNA details how the assessment was carried out. This includes:
- how the localities were determined
- the different needs of the different localities
- the different needs of people who share a particular characteristic
- a report on the PNA consultation
Necessary Services – The Pharmaceutical Regulations 2013 require the HWB to include a statement of those pharmaceutical services that it identifies as being necessary to meet the need for pharmaceutical services within the PNA. There is no definition of Necessary Services within the regulations and the HWB therefore has complete freedom in the matter.
In Bexley, once the provision of all pharmaceutical services was identified, the HWB, via the steering group, decided upon those services which were necessary to meet the pharmaceutical services for Bexley. This decision was made by service type.
Bexley HWB, through the PNA Steering Group, have decided that all Essential Services are Necessary Services in Bexley.
Other relevant services – These are services that the HWB is satisfied are not necessary to meet the need for pharmaceutical services, but their provision has secured improvements or better access to pharmaceutical services. Advanced Services for the purposes on the PNA were agreed by the Steering Group as relevant services.
To appreciate the definition of ‘pharmaceutical services’ as used in this PNA, it is important to understand the types of NHS pharmaceutical providers comprised in the pharmaceutical list maintained by the ICB on behalf of NHSE. They are:
- pharmacy contractors:
- community pharmacies
- Local Pharmaceutical Service (LPS) providers
- Distance-Selling Pharmacies (DSPs)
- Dispensing Appliance Contractors (DACs)
- dispensing GP practices
For the purposes of this PNA, ‘pharmaceutical services’ have been defined as those services that are/may be commissioned under the provider’s contract with NHSE. A detailed description of each provider type, and the pharmaceutical services as defined in their contract with NHSE, is set out below.
1.5.1 Pharmacy contractors
Pharmacy contractors comprise both those located within the Bexley HWB areas as listed in Appendix A, those in neighbouring HWB areas and remote suppliers, such as DSPs.
1.5.1.1 Community pharmacies
Community pharmacies are the most common type of pharmacy that allows the public to access their medications and advice about their health. Traditionally these were known as a chemist.
NHSE is responsible for administering opening hours for pharmacies, which is handled locally by ICBs through the delegated responsibility. A pharmacy normally has 40 core contractual hours or 72+ for those that opened under the former exemption from the control of entry test. These hours cannot be amended without the consent of the ICB. All applications are required to be considered and outcomes determined within 60 days and if approved may be implemented 30 days after approval11. This is due to change, as mentioned in Section 1.3.
It is important to clarify that under NHS community pharmacy contracts, core opening hours are contractually set at either 40 or 72 hours per week, depending on the type of contract held. Any additional hours –referred to as supplementary hours- are not mandated by the NHS and fall outside the scope of commissioned pharmaceutical services. These hours are offered at the discretion of the pharmacy contractor and, while they can improve patient access, they are delivered at the contractor’s own financial risk. Recognising the unsustainable burden this placed on the sector, the NHS took steps to reduce the 100-hour contract requirement to 72 hours and removed the 100-hour exemption from market entry regulations, acknowledging the financial and operational challenges of maintaining extended hours in an increasingly volatile environment.
This volatility has been driven by a combination of factors, including fluctuating medicine prices, dispensing at a loss and broader economic pressures affecting the sector. Many pharmacies have found it difficult to sustain extended hours under these conditions, leading to concerns about the long-term stability of service provision. While the 2025 Community Pharmacy Assurance Framework (CPAF) has introduced a degree of stability, it does not fully mitigate the financial risks associated with supplementary opening hours.
It is also essential to note that opening hours themselves are not classified as a pharmaceutical service. All NHS pharmaceutical services are delivered within the contracted 40 or 72 core hours. Integrated Care Boards (ICBs) have the remit to commission extended hours without negatively impacting the proper planning of NHS services. Such decisions should take into account the financial sustainability of community pharmacies and the potential for misalignment with broader NHS service planning -particularly as most GP practices remain closed during evenings and weekends.
There are 10,458 community pharmacies in England in September 2024 at the time of writing (this includes DSPs)12. This number has decreased from 11,071 in September 2022, when the previous PNA was published.
1.5.1.2 Distance-Selling Pharmacies (DSPs)
A DSP is a pharmacy contractor that works exclusively at a distance from patients. This includes mail order and internet pharmacies that remotely manage medicine logistics and distribution. The Pharmaceutical Regulations 2013 state that DSPs must not provide Essential Services face to face, but they may provide Advanced and Enhanced Services on the premises, as long as any Essential Service that forms part of the Advanced or Enhanced Service is not provided in person on the premises. From 1 October 2025, DSPs will no longer be able to deliver Advanced or Enhanced services face to face with patients, onsite.
As part of the terms of service for DSPs, provision of all services offered must be offered throughout England. It is therefore possible that patients within Bexley will receive pharmaceutical services from a DSP outside Bexley.
Figures for 2023-24 show that in England there were 409 DSPs13, accounting for 3.4% of the total number of pharmacies. This has increased slightly from 2020-21, when there were 372 DSPs, accounting for 3.2% of all pharmacy contractors.
1.5.1.3 Local Pharmaceutical Service (LPS) providers
A pharmacy provider may be contracted to perform specified services to their local population or a specific population group.
This contract is locally commissioned by NHSE and provision for such contracts is made in the Pharmaceutical Regulations 2013 in Part 13 and Schedule 714. Such contracts are agreed outside the national framework although may be over and above what is required from national contract. Payment for service delivery is locally agreed and funded. There are no commissioned LPS contracts in Bexley.
1.5.1.4 Pharmaceutical services
The Community Pharmacy Contractual Framework (CPCF), last agreed in 201915 is made up of three types of services:
- essential services
- advanced services
- enhanced services
Underpinning all the services is a governance structure for the delivery of pharmacy services. This structure is set out within the Pharmaceutical Regulations 2013 and includes:
- a patient and public involvement programme
- a clinical audit programme
- a risk management programme
- a clinical effectiveness programme
- a staffing and staff programme
- an information governance programme
It provides an opportunity to audit pharmacy services and to influence the evidence base for the best practice and contribution of pharmacy services, especially to meeting local health priorities within Bexley.
1.5.1.4.1 Essential Services (ES)16
Bexley has designated that all Essential Services are to be regarded as Necessary Services.
The Essential Services of the community pharmacy contract must be provided by all contractors:
- ES1: dispensing medicines – The supply of medicines and appliances ordered on NHS prescriptions, together with information and advice, to enable safe and effective use by patients and carers, and maintenance of appropriate records.
- ES2: repeat dispensing/electronic repeat dispensing – The management and dispensing of repeatable NHS prescriptions for medicines and appliances, in partnership with the patient and the prescriber.
- ES3: disposal of unwanted medicines – Acceptance, by community pharmacies, of unwanted medicines from households and individuals which require safe disposal.
- ES4: public health (promotion of healthy lifestyles) – Each financial year (1 April to 31 March), pharmacies are required to participate in up to six health campaigns at the request of NHS England. This generally involves the display and distribution of leaflets provided by NHSE. In addition, pharmacies are required to undertake prescription-linked interventions on major areas of public health concern, such as encouraging smoking cessation.
- ES5: signposting – The provision of information to people visiting the pharmacy who require further support, advice or treatment that cannot be provided by the pharmacy, on other health and social care providers or support organisations who may be able to assist them. Where appropriate, this may take the form of a referral.
- ES6: support for self-care – The provision of advice and support by pharmacy staff to enable people to derive maximum benefit from caring for themselves or their families.
- ES7: Discharge Medicines Service (DMS) – From 15 February 2021, NHS trusts are able to refer patients who would benefit from extra guidance around new prescribed medicines for provision of the DMS at their community pharmacy. The service has been identified by NHSE’s Medicines Safety Improvement Programme to be a significant contributor to the safety of patients at transitions of care, by reducing readmissions to hospital.
- ES8: Healthy Living Pharmacy (HLP) – From 1 January 2021, being a (HLP is an essential requirement for all community pharmacy contractors in England. The HLP framework is aimed at achieving consistent provision of a broad range of health promotion interventions through community pharmacies to meet local needs, improving the health and wellbeing of the local population and helping to reduce health inequalities.
- ES9: dispensing appliances – Pharmacists may regularly dispense appliances in the course of their business, or they may dispense such prescriptions infrequently, or they may have taken a decision not to dispense them at all. Whilst the Terms of Service requires a pharmacist to dispense any (non-Part XVIIIA listed) medicine “with reasonable promptness”, for appliances the obligation to dispense arises only if the pharmacist supplies such products “in the normal course of business”.
Both Essential and Advanced Services provide an opportunity to identify issues with side effects or changes in dosage, confirmation that the patient understands the role of the medicine or appliance in their care, and opportunities for medicine optimisation. Appropriate referrals can be made to GPs or other care settings, resulting in patients receiving a better outcome from their medicines and, in some cases, cost-saving for the commissioner.
1.5.1.4.2 Advanced Services (AS)17
Advanced Services are all considered relevant for the purpose of this PNA.
There are nine Advanced Services within the CPCF. Advanced Services are not mandatory for providers to provide and therefore community pharmacies can choose to provide any of these services as long as they meet the requirements set out in the Secretary of State Directions. The Advanced Services are listed below and the number of pharmacy participants for each service in Bexley can be seen in Section 3.2.4 and in Section 6.2 by locality.
- AS1: Pharmacy First service – The Pharmacy First service builds upon the NHS Community Pharmacist Consultation Service (CPCS) which has run since October 2019 and enabled patients to be referred into community pharmacy for a minor illness or an urgent repeat medicine supply. The new Pharmacy First service, launched 31 January 2024, adds to the Consultation Service and enables community pharmacies to provide care for seven common conditions following defined clinical pathways. The initiative encourages patients to obtain treatment for the conditions directly from community pharmacies without needing a GP appointment. These conditions are sinusitis, sore throat, earache, infected insect bites, impetigo, shingles, and uncomplicated urinary tract infections in women. Pharmacists can now provide prescription-only medicines, including antibiotics and antivirals, where clinically appropriate, after a consultation held in a private consultation room or area. More than 10,000 pharmacies, covering over 95% of England, have signed up to Pharmacy First and patients can find their nearest pharmacy offering the service online. An improvement requested by GP practices is to remove any need for a referral from a GP practice to the service and allow all patients, both minor illness and common conditions, to self-refer to a pharmacy with appropriate remuneration arrangements in place.
- AS2: Flu Vaccination service – A service to sustain and maximise uptake of flu vaccine in at-risk groups by providing more opportunities for access and improve convenience for eligible patients to access flu vaccinations. This service is commissioned nationally.
- AS3: Pharmacy Contraception Service (PCS) – The PCS started on 24 April 2023, allowing the on-going supply of Oral Contraception (OC) from community pharmacies. From 1 December 2023, the service included both initiation and on-going supply of OC. The supplies are authorised via a PGD, with appropriate checks, such as the measurement of the patient’s blood pressure and body mass index, being undertaken, where necessary. From October 2025 the Pharmacy Contraception Service (PCS) will be expanded to include Emergency Hormonal Contraception.
- AS4: Hypertension case-finding service – This service was introduced in October 2021. The service has two stages – the first is identifying people at risk of hypertension and offering them blood pressure measurement (a ‘clinic check’). The second stage, where clinically indicated, is offering ambulatory blood pressure monitoring. The blood pressure and ambulatory blood pressure monitoring results will then be shared with the GP practice where the patient is registered to inform a potential diagnosis of hypertension.
- AS5: New Medicine Service (NMS) – The service provides support to people who are prescribed a new medicine to manage a long-term condition, which will generally help them to appropriately improve their medication adherence and enhance self-management of the long-term condition. Specific conditions/medicines are covered by the service. New Medicine Service will be expanded to include depression from October 2025.
- AS6: Smoking Cessation Service (SCS) – This service is commissioned as an Advanced service from 10 March 2022. It enables NHS trusts to refer patients discharged from hospital to a community pharmacy of their choice to continue their smoking cessation care pathway, including providing medication and behavioural support as required, in line with the NHS LTP care model for tobacco addiction.
- AS7: Appliance Use Review (AUR) – To improve the patient’s knowledge and use of any ‘specified appliance’ by:
- establishing the way the patient uses the appliance and the patient’s experience of such use
- identifying, discussing and assisting in the resolution of poor or ineffective use of the appliance by the patient
- advising the patient on the safe and appropriate storage of the appliance
- advising the patient on the safe and proper disposal of appliances that are used or unwanted
- AS8: Stoma Appliance Customisation (SAC) – This service involves the customisation of a quantity of more than one stoma appliance, based on the patient’s measurements or a template. The aim of the service is to ensure proper use and comfortable fitting of the stoma appliance and to improve the duration of usage, thereby reducing waste.
- AS9: LFD service – The Lateral flow device tests supply service for patients potentially eligible for COVID-19 treatments (LFD service) is commissioned as an Advanced service from 6 November 2023. The objective of this service is to offer eligible at-risk patients access to LFD tests to enable testing at home for COVID-19, following symptoms of infection. A positive LFD test result will be used to inform a clinical assessment to determine whether the patient is suitable for and will benefit from NICE recommended COVID-19 treatments.
1.5.1.4.3 Enhanced Services18
Enhanced Services are all considered relevant for the purpose of this PNA.
Under the pharmacy contract, National Enhanced Services (NES) are those directly commissioned by NHS England (NHSE) as part of a nationally coordinated programme. There are currently two National Enhanced Services commissioned, one is currently being provided, and the other one is undergoing national procurement.
- NES1: COVID-19 vaccination service: This service is provided from selected community pharmacies who have undergone an Expression of Interest Process and commissioned by NHSE. Pharmacy owners must also provide the Flu Vaccination Service and is provided for a selected cohort of patients.
- NES2: Respiratory Syncytial Virus (RSV) vaccination and Pertussis vaccination service: currently under procurement, is due to go live in autumn 2025.
Local Enhanced Services (LES) are developed and designed locally by NHS England, in consultation with Local Pharmaceutical Committees (LPCs), to meet local health needs. There are four services commissioned regionally by NHS London as coordinated by the Dentistry, Optometry and Pharmacy Commissioning Hub or by the North East London ICB on behalf of all London ICBs through the delegated authority by NHSE.
- LES1: Bank Holiday service: provides coverage over Bank Holidays, Easter Sunday, and Christmas Day, to ensure that there are pharmacies open on these days so patients can access medication if required.
- LES2: Measles, Mumps and Rubella (MMR) vaccination service: pharmacies are commissioned by direct award based on areas of low uptake and proven experience and success of running similar schemes. This service is commissioned to deliver by the currently selected sites until end of March 2026.
- LES3: Pneumococcal Polysaccharide Vaccine (PPV) service: was issued in April 2025 as currently commissioned. Pharmacies can sign up to provide this service.
- LES4: London Flu: the specification for this vaccination service is currently being drawn up for 2025/26 and will come into effect from 1 September 2025. Pharmacies that are already providing the national Flu advanced service can sign up to provide this local service. The London Flu service runs in parallel to the national Flu programme, with cohorts that sit outside of the Flu advanced service as described in Section 1.5.1.4.2.
1.5.1.5 Pharmacy Access Scheme (PhAS) providers19
The PhAS has been designed to capture the pharmacies that are most important for patient access, specifically those pharmacies where patient and public access would be materially affected should they close. The PhAS takes isolation and need levels into account.
Pharmacies in areas with dense provision of pharmacies remain excluded from the scheme. In areas with high numbers of pharmacies, public access to NHS pharmaceutical services is not at risk. The scheme is focused on areas that may be at risk of reduced access, for example, where a local population relies on a single pharmacy.
DSPs, DACs, LPS contractors and dispensing GP practices are ineligible for the scheme.
From 1 January 2022, the revised PhAS is to continue to support patient access to isolated, eligible pharmacies and ensure patient access to NHS community pharmaceutical services is protected.
1.5.1.6 Other services
As stated in Section 1.4, for the purpose of this PNA ‘pharmaceutical services’ have been defined as those which are or may be commissioned under the provider’s contract with NHSE.
Section 4 outlines services provided by NHS pharmaceutical providers in Bexley commissioned by organisations other than NHSE or provided privately, and therefore out of scope of the PNA. At the time of writing the commissioning organisations primarily discussed are the local authority and ICB.
1.5.2 Dispensing Appliance Contractors (DACs)
DACs operate under the Terms of Service for Appliance Contractors as set out in Schedule 5 of the Pharmaceutical Regulations 2013. They can supply appliances against an NHS prescription such as stoma and incontinence aids, dressings, bandages etc. They are not required to have a pharmacist, do not have a regulatory body and their premises do not have to be registered with the General Pharmaceutical Council.
DACs must provide a range of Essential Services such as dispensing of appliances, advice on appliances, signposting, clinical governance and home delivery of appliances. In addition, DACs may provide the Advanced Services of AUR and SAC. As of June 202420 there were a total of 111 DACs in England.
Pharmacy contractors, dispensing GP practices and LPS providers may supply appliances, but DACs are unable to supply medicines.
1.5.3 Dispensing GP practices
The Pharmaceutical Regulations 2013, as set out in Part 8 and Schedule 6, permit GPs in certain areas to dispense NHS prescriptions for defined populations.
These provisions are to allow patients in rural communities, who do not have reasonable access to a community pharmacy, to have access to dispensing services from their GP practice. Dispensing GP practices therefore make a valuable contribution to dispensing services although they do not offer the full range of pharmaceutical services offered at community pharmacies. Dispensing GP practices can provide such services to communities within areas known as ‘controlled localities’.
GP premises for dispensing must be listed within the pharmaceutical list held by NHSE and patients retain the right of choice to have their prescription dispensed from a community pharmacy if they wish.
1.5.4 Other providers of pharmaceutical services in neighbouring areas
There are three other HWBs that border Bexley, two of them are also in London:
- Bromley HWB
- Greenwich HWB
- Kent HWB
In determining the needs for pharmaceutical service provision to the population of Bexley, consideration has also been made to the pharmaceutical service provision from the neighbouring HWB areas.
1.6 Process for developing the PNA
Bexley HWB has statutory responsibilities under the Health and Social Care Act to produce and publicise a revised PNA at least every three years. The last PNA for Bexley was published in September 2022 and is therefore due to be reassessed and published by end of September 2025.
Public Health in the London Borough of Bexley (LBB) has a duty to complete the PNA on behalf of the Bexley HWB, and they commissioned Soar Beyond Ltd to undertake the Bexley PNA 2025.
- Step 1: project set up and governance established between LBB Public Health and Soar Beyond Ltd.
- Step 2: steering group – On 5 July 2024 Bexley PNA Steering Group was established. The terms of reference and membership of the group can be found in Appendix C.
- Step 3: project management – At this first meeting, Soar Beyond Ltd and the local authority presented and agreed the project plan and ongoing maintenance of the project plan. Appendix B shows an approved timeline for the project.
- Step 4: review of existing PNA and JSNA – Through the project manager, the PNA Steering Group reviewed the existing PNA and JSNA.
- Step 5a: public questionnaire on pharmacy provision – A public questionnaire to establish views about pharmacy services was agreed by the Steering Group and circulated to residents via various channels. A total of 401 responses were received. A copy of the public questionnaire can be found in Appendix D with detailed responses.
- Step 5b: pharmacy contractor questionnaire – The Steering Group agreed a questionnaire to be distributed to the local community pharmacies to collate information for the PNA. There were only nine responses, making it challenging to draw meaningful conclusions. The steering group agreed not to use the limited data for analysis but to document the engagement attempt in the PNA, acknowledging the challenges faced by community pharmacies which most likely would have been a contributing factor to the low response.
- Step 6: mapping of services – Details of services and service providers were collated and triangulated to ensure the information that the assessment was based on was the most robust and accurate. The Pharmacy Contracting function within the ICB, as the commissioner of service providers and services classed as necessary and relevant, was predominantly used as a base for information due to its contractual obligation to hold and maintain pharmaceutical lists on behalf of NHSE. Information was collated, ratified and shared with the Steering Group before the assessment was commenced. The pharmaceutical list dated 1 November 2024 was used for the draft assessment.
- Step 7: preparing the draft PNA for consultation – The Steering Group reviewed and revised the content and detail of the draft PNA. The process took into account the demography, health needs of residents in the local area, JSNA and other relevant strategies in order to ensure the priorities were identified correctly. As the PNA is an assessment taken at a defined moment in time, the Steering Group agreed to monitor any changes and, if necessary, to update the PNA before finalising or publish with accompanying supplementary statements as per the regulations, unless the changes had a significant impact on the conclusions. In the case of the latter, the Steering Group were fully aware of the need to reassess.
- Step 8: consultation – In line with the Pharmaceutical Regulations 2013, a consultation on the draft PNA was undertaken between 10 February and 13 April 2025. The draft PNA and consultation response form was issued to all identified stakeholders. These are listed in the final PNA in Appendix E.
- Step 9: collation and analysis of consultation responses – The consultation responses were collated by the council and analysed by the Steering Group. A summary of the responses received is noted in Appendix F, and full comments are included in Appendix G.
- Step 10: review of all pharmaceutical list notifications – The steering group reviewed all amendments made since the draft PNA and concluded that these changes did not alter the overall findings. The section on pharmaceutical service provision was therefore updated in June 2025 to reflect the most accurate information available at the time of publication.
- Step 11: production of final PNA – future stage – The collation and analysis of consultation responses was used by the project manager to revise the draft PNA, and the final PNA was presented to the PNA Steering Group. The final PNA was signed off by the Director of Public Health and subsequently published on the council’s website.
1.7 Localities for the purpose of the PNA
The PNA Steering Group, at its first meeting, considered how the localities within Bexley geography would be defined.
The majority of health and social care data is available at Local Authority (LA) council ward level and at this level provides reasonable statistical rigour. It was agreed that the council wards would be used to define the localities of the Bexley HWB geography.
The localities and wards used for the PNA for Bexley HWB area are:
| Locality | Wards |
|---|---|
| North Bexley | Barnehurst, Belvedere, Crayford, Erith, Northumberland Heath, Slade Green & Northend, Thamesmead East |
| Clocktower | Bexleyheath, Crook Log, East Wickham, Falconwood & Welling, West Heath |
| Frognal | Blackfen & Lamorbey, Blendon & Penhill, Longlands, Sidcup, St Mary’s & St James |
The three localities are co-terminus with the identified wards listed in the table above. The determination of these localities is based on proven experience of former Bexley PNA where the three localities were identified. This divides Bexley into three distinct localities.
Figure 1 shows the split of localities across Bexley and figure 2 shows the wards' divisions therein.
A list of providers of pharmaceutical services is found in Appendix A.
The information contained in Appendix A has been provided by South East London (SEL) ICB and the LBB. Once collated, it was ratified by the steering group during the second steering group meeting.
Figure 1: Map to show the localities in Bexley
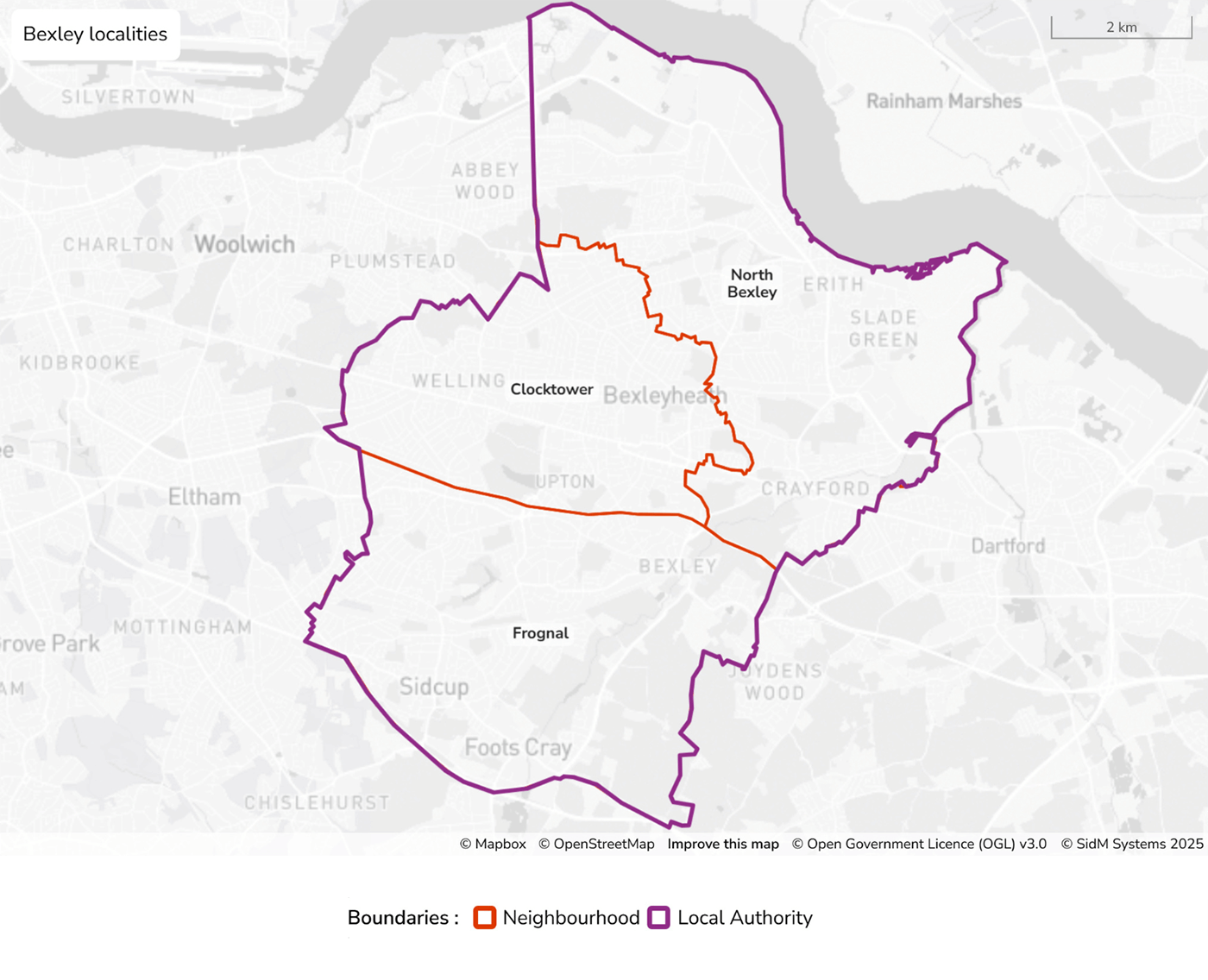
Figure 1 - text description
- This map displays the London Borough of Bexley in southeast London, highlighting both local authority and locality boundaries. The borough boundary is marked with a purple line, while the Clocktower neighbourhood, located centrally within Bexley, is outlined in orange. Other labeled localities within the borough include North Bexley in the north and Frognal in the south. Surrounding areas outside the borough, such as Woolwich, Eltham, Mottingham, Chislehurst, and Dartford, are also visible but not enclosed within the purple line. The river Thames conforms the border in the north.
Figure 2: Map showing the localities and wards in Bexley
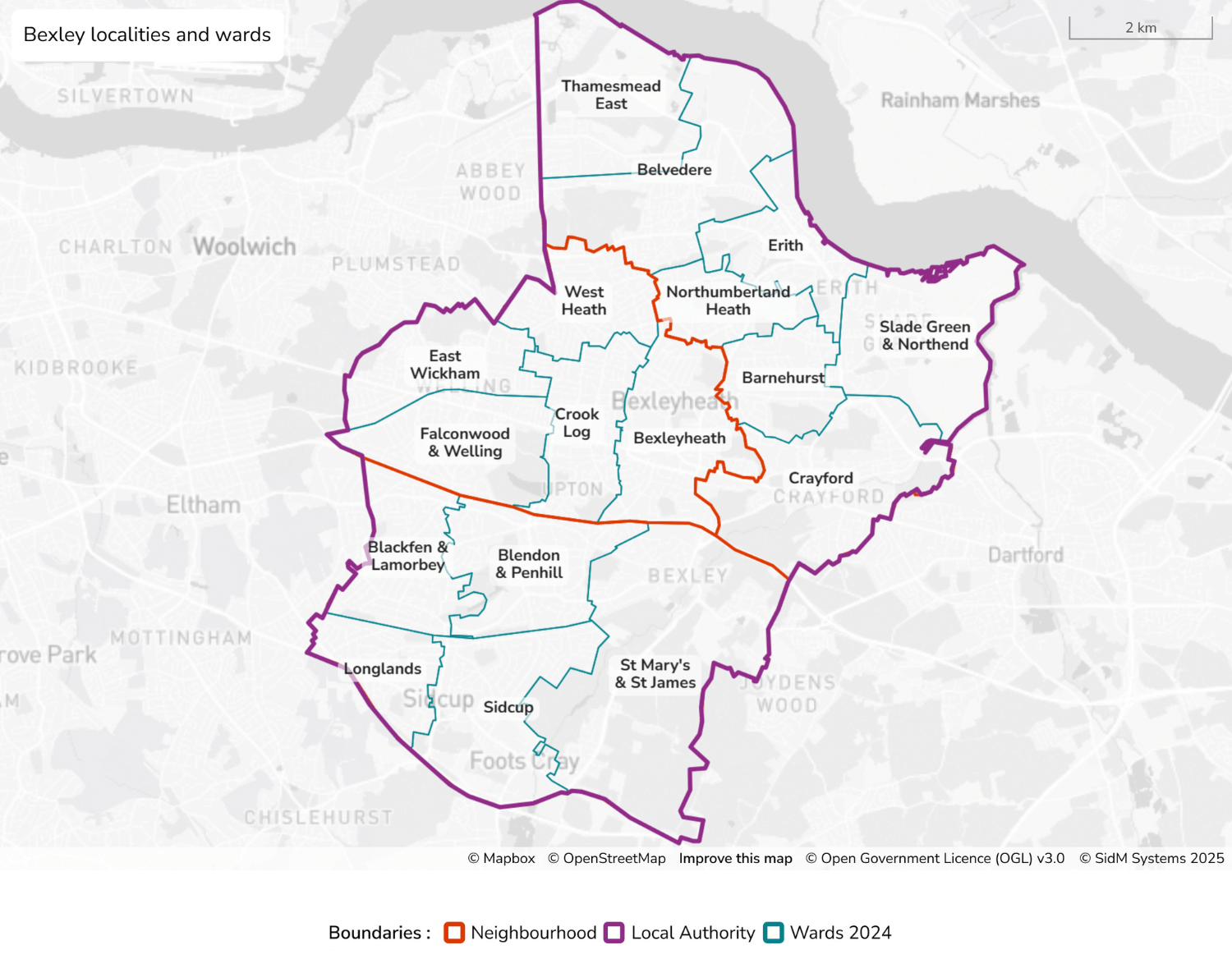
Figure 2 - text description
- This map illustrates the London Borough of Bexley, showing detailed administrative divisions including the borough, localities and 2024 ward boundaries. The borough boundary is marked with a thick purple line, enclosing all of Bexley. The localities of North Bexley, Clocktower and Frognal are outlined in orange. In addition, multiple wards, each outlined in light blue, represent electoral divisions as of 2024. In the north near the River Thames: Thamesmead East, Belvedere, Erith, Northumberland Heath, and Slade Green & Northend. In the central and west areas: West Heath, East Wickham, Falconwood & Welling, Crook Log, Bexleyheath, Barnehurst, and Crayford. In the south: Blackfen & Lamorbey, Blendon & Penhill, Sidcup, Longlands, and St Mary’s & St James. Surrounding areas beyond Bexley's boundaries include Woolwich, Eltham, Dartford, Chislehurst, and Mottingham, which are shown in grey without boundary lines, indicating they are outside the borough. The River Thames defines Bexley’s northern edge, with Rainham Marshes across the river.
2 InPharmacy. NPA warns that pharmacy closures are at record high levels May 2024
3 Healthwatch. Pharmacy closures in England. September 2024
4 Community Pharmacy England. Pharmacy Pressures Survey November 2024
5 Community Pharmacy England. Pharmacy First Service November 2024
6 Community Pharmacy England. Hypertension Case-Finding Service July 2024
7 Community Pharmacy England. LFD Service August 2024
8 NHSE. Pharmacy Quality Scheme: Guidance 2023/24 September 2024
9 London Borough of Bexley (LBB). Bexley Data Observatory
10 LBB. Bexley Joint Local Health and Wellbeing Strategy 2023 to 2028
11 Community Pharmacy England. Changing Core Opening Hours June 2024
13 NHSBA. General Pharmaceutical Services in England 2015-16 to 2023-24 October 2024
16 Community Pharmacy England. Essential Services April 2024
17 Community Pharmacy England. Advanced Services February 2024
18 Community Pharmacy England. National Enhanced Services November 2024
